OpenEMR 6.x Billing - Claims Workflows
...this page might be under construction for the next few days... Billing: Submit Claims
Introduction
OpenEMR's billing module is an integrated set of many functionalities that handle all the aspects of billing that OpenEMR provides. This document only shows the claims- related activities.
Being as comprehensive as they are, the claims workflows depend on settings and data from other parts of the EMR in order to fulfill their missions. Those requirements will not be detailed here, but they do need to be properly in place for claims to be successfully processed.* Be sure the Facility and Practice settings; Patient demographics and insurance information are correct [[List_of_OpenEMR_Data_Fields_Required_For_Insurance_Claims]]
- The encounter(s) to be billed must be complete; see [[HOWTO:_Create_A_Claim-_Ready_Encounter]]
- And, of course, the practice must have an account with a compatible clearinghouse
OpenEMR's Billing Manager can generate either x12 claim batch files for electronic claim submission, and HCFA claim forms for postal mailing to the payer. X12 files are automatically saved to the designated download directory or folder of the billing user's browser, from where they may be uploaded to a clearinghouse. HCFA forms are saved as text or PDFs to that same download location, from where they may be sent to a printer attached to the billing user's computer. The workflows for both X12 and HCFA claim files are nearly the same; the variations will be mentioned at the appropriate places in the instructions below.
The entire claim workflow can be divided into five major steps which will be divided into the following two wiki pages:
Page 1, Billing: Submit Claims - this wiki page
- Step 1. Generate Claims In OpenEMR
- Step 2. Upload To Clearinghouse
- Step 3. Check For Response Files
Page 2, OpenEMR 6.x Billing: Process Payments
- Step 4. Download Response Files
- Step 5. Apply Payments
Note: Most screenshots were taken on an OpenEMR v6.0(3) install but new interface changes are anticipated soon so more modern versions may look slightly different.
Billing - Submit Claims
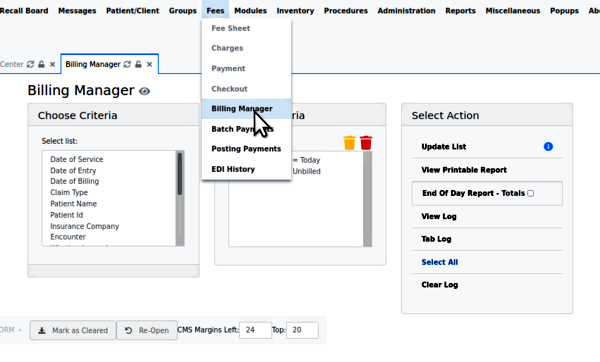
Having in place all the prerequisites mentioned above, the claims submission process all begins here: from the OpenEMR main menu, click 'Fees/ Billing Manager'; see the opening screen.
Note: unlike many OpenEMR functions, the Billing Manager may be operated without a patient record open.
Step One: Generate Claims In OpenEMR
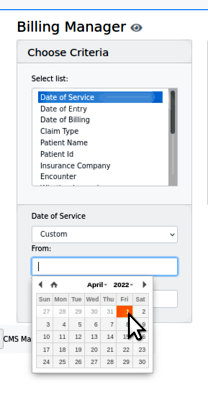
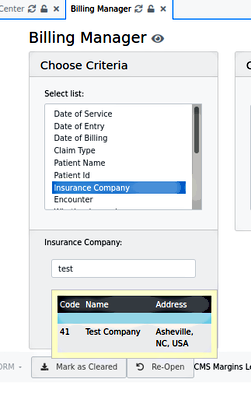
1. Search for the claims - the search criteria will open different types of smaller panels in which to specify the search terms:
- All date criteria have date pickers
- The list- formatted data will show what has been configured in the EMR. See here the insurance company provided by 'Practice Settings/ Insurance Companies'
- Any simple text criteria will merely have a text input area (not pictured)
- Any simple text criteria will merely have a text input area (not pictured)
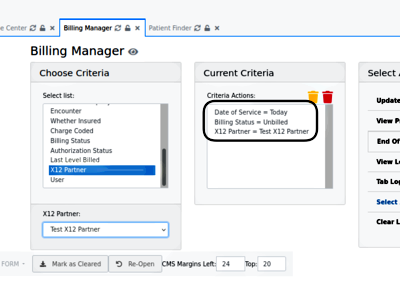
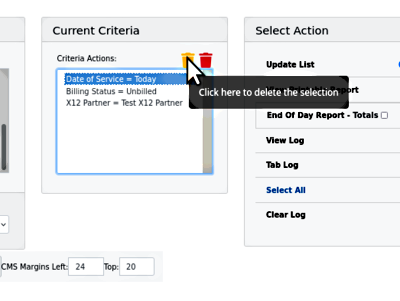
As they are input, the search terms are added to 'Current Criteria' (round rectangle)
If you want to remove any terms from the Current Criteria, the yellow trash can deletes the selected one (here, Date of Service);
...the red can deletes them all.
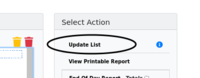
2. Click 'update list' to generate the list of claims
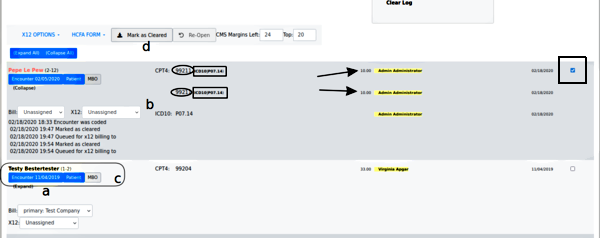
Find the following lettered items in the picture below
- a. look in the 'Expand' link to see the claim history (the display opens up, as Pepe's item shows)
Note: a red patient name (e.g., Pepe's) means something is wrong in insurance info... his has no insurance company selected.
- b. check that each claim has all the required elements:
- both the 'Bill' (insurance) and 'X12' dropdowns are selected
- the CPT4 or other service code (oval) given for the service(s) rendered in that encounter
- the justifying ICD10 diagnosis code (rectangle) for each CPT code
- the fee (arrow) for each CPT code
- the rendering provider (yellow highlight) for each line item
- Date of Service
- c. each claim component may be edited from this claim listing
- click on 'encounter' to open the encounter summary form to fix things wrong with the encounter/ fee sheet
- click on 'Patient' for demographics or insurance company information errors
- d. you can reopen claims that have been marked as billed but not yet submitted
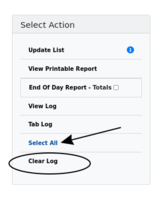
3. Click 'Clear Log' (oval below) before validating this batch of claims
4. Select specific claims (individual checkbox, at far right in Pepe's claim, above) or 'Select All' (arrow in previous pic)
5. Generate the claim printout files
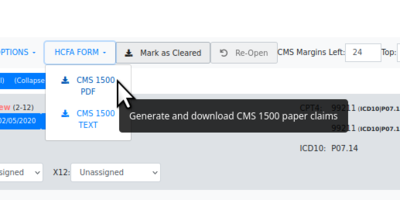
- HCFA claims - Click the 'HCFA FORM' dropdown
- then select desired claim file format, .txt or .pdf
- The file will be saved in the browser's designated local download location.
- The data is laid out on the page to fit into the text areas on the HCFA claim form
- It may be sent to a printer which has been loaded with the pre- printed HCFA forms.
- X12 claims -
- Generate the claim batch file:
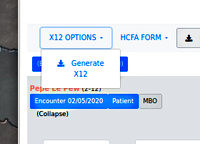
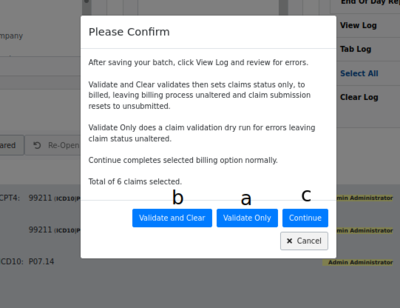
Find the lettered items below in the following picture
- a. First: click 'X12 Options', 'Generate X12' then 'Validate Only'
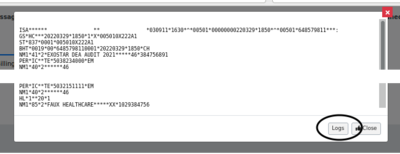
- The X12 file displays.
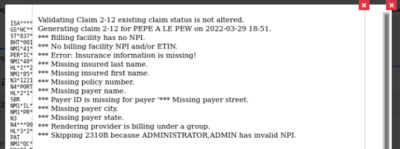
... then click 'Logs' at the bottom (oval lower right) to see if the validation log has errors
The validation log is another place to find what errors exist in the claim file that will prevent it from being accepted.
- Claims with errors may be either corrected from the claim list and re- validated til clear of errors, or simply unselected from the list. That claim will be excluded from the batch file but will re-appear next time a search is done that includes it.
To finish the claim generation process:
- b. click 'X12 Options' again, 'Generate X12' then 'Validate and Clear' (no need to check the logs, you just fixed everything)
- c. click 'X12 Options'/ 'Generate X12'/ 'Continue'
- to obtain the batch file (not pictured; is a simple file download dialog)
- or to automatically upload it to clearinghouse if SFTP is configured.
Step Two: Upload To Clearinghouse
This step varies widely depending on the clearinghouse. They all have similar functionalities because they're performing the same task but the mechanics differ significantly.* As mentioned, if an SFTP connection is being used, when the 'X12 Options/ Continue' button is clicked the transfer to the clearinghouse will happen automatically and a message to that effect will be displayed (not pictured).
- Otherwise, the claim files need to be uploaded manually, typically through a web portal of some sort.
- I (author HT) have worked with Trizetto, Availity and Office Ally. I personally found Office Ally to be the least versatile in the services they offer but also the least difficult to learn and to work with. The other two are much more full- featured services but their customer interaction interface is exceedingly complex, especially in interpreting response files.
Step Three: Check For Response Files
All clearinghouses will return some sort of response files to tell you the status of the claims in the uploaded batch file(s). But since their methods are so different from each other we won't get into any of them here; your billing or IT consultant will need to learn the idiosyncrasies.
- Generally, claim files will be rejected by the clearinghouse for incompatibility reasons, e.g., malformed x12 claim files (data missing or placed in the wrong fields).
- After it is accepted by the clearinghouse the claim file may be rejected by the payer for claim data problems, e.g., a patient's policy was not in effect on the Date Of Service.
- In either case you may correct the error and resubmit the claim.
- a. Go back to first section above, (step 1) and search on the corrected claim
- b. select it from the results (arrow at right below), click 'Re-open' (oval)
- c. include it in a future outgoing batch file
- Once the claim is accepted by the payer they will eventually send an ERA file with the payment
NEXT section: Billing: Process Payments]